Items filtered by date: September 2023
Causes and Prevention of Athlete’s Foot

Athlete's foot, a common fungal infection of the skin on the feet, can cause discomfort and itching, making it essential to understand its causes and preventive measures. This contagious infection thrives in warm, moist environments, making sweaty feet or damp socks and shoes prime breeding grounds. Walking barefoot in public places such as locker rooms, swimming pool areas, or communal showers increases the risk of exposure to the fungus. Sharing towels, shoes, or socks with an infected person can also facilitate its spread. Certain factors can make individuals more susceptible to athlete's foot, such as compromised immune systems, diabetes, or excessive sweating. To prevent this bothersome condition, it is helpful to maintain good foot hygiene by washing and drying your feet thoroughly, especially between the toes. Keep feet dry and avoid tight, non-breathable shoes. If you suspect you have athlete's foot, it is suggested that you consult a podiatrist for prompt treatment to prevent further complications and the spread of the infection.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with one of our podiatrists from Florida Family Podiatry. Our doctors will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our offices located in Delray Beach and Boynton Beach, FL. . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Keep Your Feet Healthy So You Can Stay Active
Surgery for Morton’s Neuroma
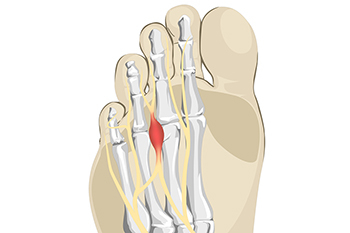
Morton's neuroma is a condition affecting the plantar digital nerve and is common in middle-aged women. Surgical excision is recommended when conservative treatments fail. Various surgical approaches exist, with dorsal and plantar accesses being the most common. Regenerative surgery uses platelet-rich plasma, or PRP, for complications arising from Morton's neuroma surgery. PRP is derived from the patient's own blood. It contains growth factors that aid in tissue healing. Hyaluronic acid acts as a platform for PRP, promoting tissue regeneration and reducing healing time. The combinations of these things offer a valuable technique that promotes complete wound healing, with satisfactory aesthetic and functional outcomes. If you have a Morton’s neuroma that requires surgical intervention, it is suggested that you make an appointment with a podiatrist to discuss whether PRP and HA can be used in the surgery to help with recovery.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Florida Family Podiatry. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Delray Beach and Boynton Beach, FL. . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Pressure Ulcers on the Feet

Pressure ulcers are a significant concern in healthcare. These wounds develop due to prolonged pressure on the skin, often affecting individuals with limited mobility or those with underlying health conditions. Pressure ulcers can also result from reduced blood flow to the skin. Any break in the skin caused by pressure can lead to infection. Common infections related to pressure ulcers include localized infections, cellulitis, and osteomyelitis, which can progress to sepsis, a life-threatening condition. Prolonged pressure reduces blood flow to the skin, which can result in tissue damage. Foot pressure ulcers often occur on bony prominences such as the heels and ankles. People using improperly fitted prosthetics, those who wear shoes that rub on various parts of the foot, and people with fragile skin are more susceptible to these wounds. Early detection and treatment are essential for better outcomes. Daily foot checks can help detect pressure ulcers and result in timely intervention. If the skin breaks, vigilance should be practiced for signs of infection, such as pus, foul odor, and increased redness. Once a pressure ulcer forms, treatment includes wound cleaning, protection from pressure, and other medical care depending on the severity of the ulcer. If you have a foot wound, it is strongly suggested that you make an appointment with a podiatrist as quickly as possible for treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Florida Family Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Delray Beach and Boynton Beach, FL. . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Dealing With Lisfranc Injuries

Lisfranc injuries, though rare, can have debilitating consequences if not properly managed. These acute and traumatic injuries affect the tarsometatarsal joints in the midfoot, ranging from mild sprains to severe dislocation fractures. These joints help to transfer force between the rearfoot and forefoot during walking. Recognizing Lisfranc injuries involves noting diffuse pain, swelling, and inability to bear weight around the midfoot. The pain peaks when the midfoot becomes a rigid lever for weight transfer. Dismissing these injuries as mere bruising can lead to complications like post-traumatic arthritis and chronic pain. Staying off the foot, stability, and strengthening can lead to recovery. Exercises and orthotics can also help. Treatment may include wearing a special boot and controlled weight bearing. Lisfranc injuries are complex but manageable. To regain proper mobility and prevent long-term complications from Lisfranc injuries in the foot, it is suggested that you visit a podiatrist for a diagnosis and treatment plan.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact one of our podiatrists from Florida Family Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our offices located in Delray Beach and Boynton Beach, FL. . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.